It is deeply concerning to learn about the significant increase in syphilis cases among newborns, as reported by the U.S. health officials.
The surge in congenital syphilis cases, with more than 3,700 babies affected in 2022, is indeed alarming. The fact that this number is ten times higher than a decade ago and represents a 32% increase from the previous year is a cause for serious concern.
The impact of syphilis on newborns is further highlighted by the distressing statistic that it led to 282 stillbirth and infant deaths in 2022, a figure nearly 16 times higher than the deaths recorded in 2012.
These figures underscore the urgent need for enhanced preventive measures to address this public health issue.
The Centers for Disease Control and Prevention’s revelation that the 2022 count of congenital syphilis cases was the highest in over 30 years is a stark reminder of the gravity of the situation.
Equally distressing is the fact that in more than half of the cases, the mothers tested positive for syphilis during pregnancy but did not receive appropriate treatment.
In light of these troubling statistics, it is imperative that comprehensive and targeted measures are implemented to address the rising incidence of congenital syphilis.
Encouraging millions of women of childbearing age and their partners to undergo testing for this sexually transmitted disease is a critical step in preventing its transmission to newborns.
Additionally, ensuring that expectant mothers who test positive for syphilis receive timely and effective treatment is essential in safeguarding the health and well-being of both the mother and the unborn child.
The implications of these findings are far-reaching, and it is incumbent upon healthcare authorities, policymakers, and the broader community to work collaboratively to tackle this pressing public health issue.
By prioritizing education, access to testing, and timely intervention, we can strive to reverse the disturbing trend of congenital syphilis cases and protect the health of future generations.
In conclusion, the escalating prevalence of congenital syphilis demands urgent and concerted action.
By raising awareness, promoting testing, and ensuring access to appropriate healthcare services, we can endeavor to mitigate the impact of this concerning trend and safeguard the well-being of newborns and their families.
The alarming increase in cases of congenital syphilis is a cause for great concern, particularly in light of the repeated warnings issued by public health agencies.
The surge in primary and secondary cases of syphilis in adults has undoubtedly played a significant role in this rise, as highlighted by officials from the Centers for Disease Control and Prevention (CDC).
Furthermore, the shortage of benzathine penicillin injections, which are the primary medical treatment for congenital syphilis, has only exacerbated the situation.
This shortage has posed a significant challenge for medical providers, who are struggling to access the necessary medication to effectively combat this growing public health issue.
The combination of these factors underscores the urgent need for comprehensive and coordinated efforts to address the resurgence of congenital syphilis and its associated complications.
It is imperative that stakeholders at all levels work together to address the root causes of this troubling trend and ensure that adequate resources and support are available to prevent and treat congenital syphilis.
The recent surge in syphilis cases among newborns has prompted a call to action from the Centers for Disease Control and Prevention (CDC). Dr. Laura Bachmann of the CDC emphasized the urgent need for significant changes to address this distressing epidemic.
It is evident that the current approach is not effectively curbing the spread of syphilis, and proactive measures are imperative.
The CDC has proposed several key strategies to combat the escalating rates of congenital syphilis. One of the primary recommendations is to initiate syphilis treatment as soon as a pregnant woman tests positive, without waiting for confirmatory testing.
Additionally, the CDC advocates for improved access to transportation to ensure that women can promptly receive the necessary treatment.
Furthermore, the CDC urges the expansion of rapid testing beyond traditional healthcare settings to locations such as emergency rooms, needle-exchange programs, prisons, and jails.
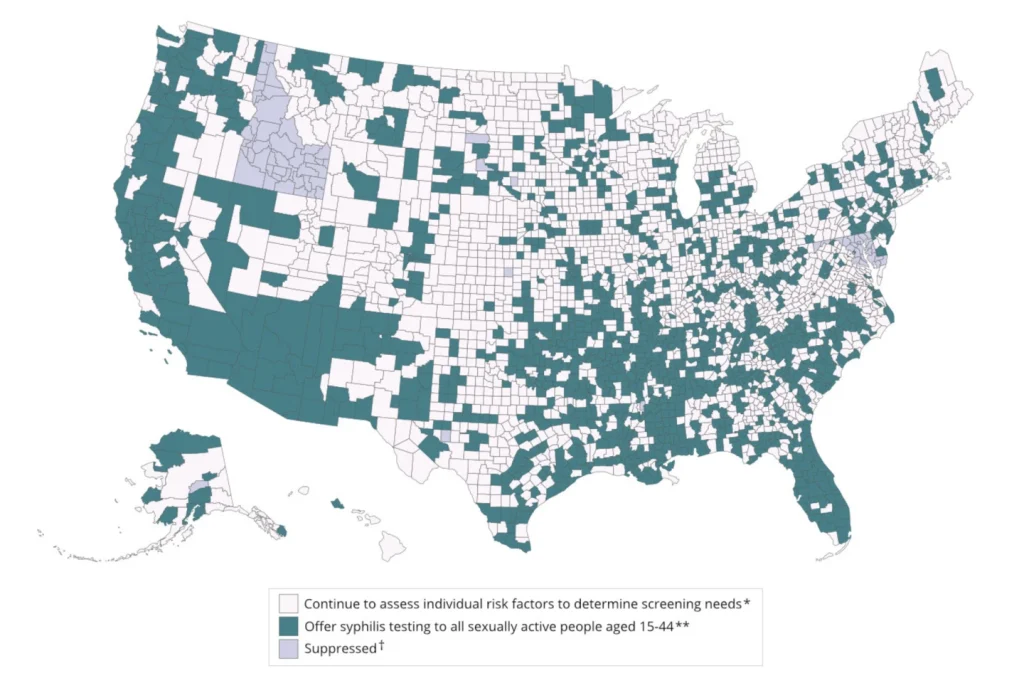
In light of the concerning statistics, the CDC has reiterated the importance of regular syphilis testing for sexually active women of childbearing age and their partners, particularly in areas with high prevalence.
According to the CDC’s new map and definition, approximately 70% of adults in the United States reside in counties with elevated syphilis rates, potentially affecting tens of millions of individuals.
It is crucial to note that while the CDC has issued these recommendations, there is no additional federal funding allocated to support state and local health departments in implementing these measures.
Several state health departments have expressed concerns about resource constraints in terms of treatment and prevention efforts.
However, there have been positive developments, such as Illinois launching a dedicated phone line to assist healthcare providers with record searching, consultation, and mandatory reporting.
In conclusion, the CDC’s call for exceptional measures underscores the urgency of addressing the escalating rates of congenital syphilis.
It is imperative for stakeholders at all levels to collaborate and take proactive steps to implement these recommendations and allocate the necessary resources to combat this distressing epidemic effectively.
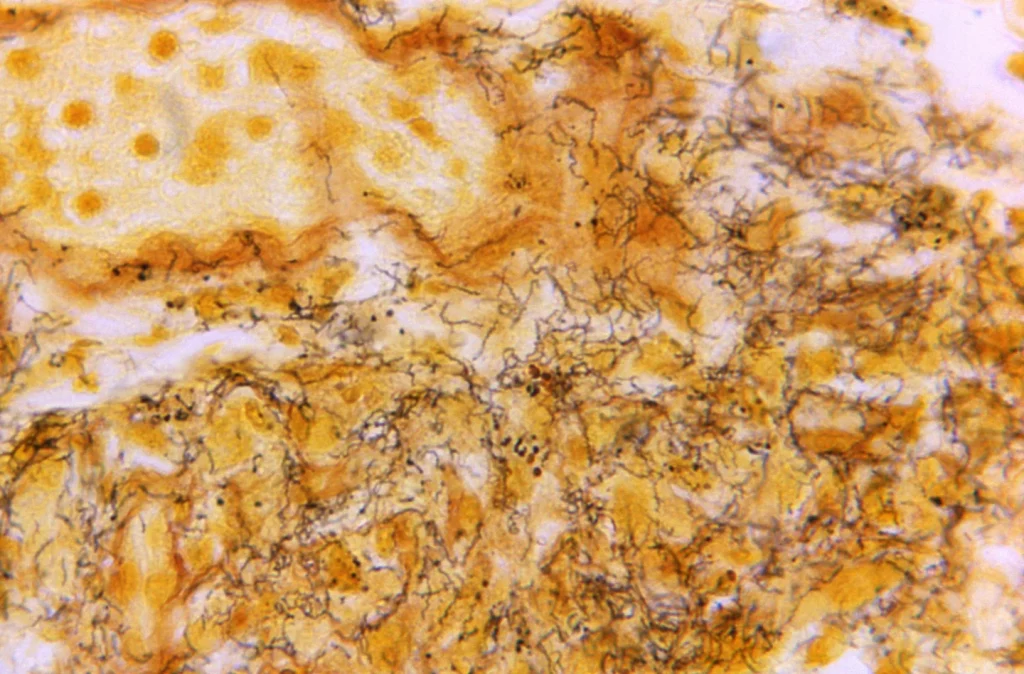
Syphilis, a bacterial infection that has been a common and feared sexually transmitted disease for centuries, saw a significant decrease in new infections in the United States in the 1940s with the widespread availability of antibiotics.
However, by the late 1990s, cases began to rise again, with men who have sex with other men being disproportionately affected.
This STD is now spreading among several demographics, and case rates have been rising across racial and ethnic groups.
In cases of congenital syphilis, mothers can pass the disease on to their babies, potentially leading to the death of the child or health problems such as deafness, blindness, and malformed bones.
Dr. Mike Saag, an infectious diseases expert at the University of Alabama at Birmingham, emphasized that syphilis can be a “silent infection” in women, as it is difficult to diagnose without a blood test, and not everyone experiences painless sores or other visible symptoms.
The CDC has long recommended that all pregnant women should be tested for syphilis at their first prenatal visit, but poor access to prenatal care in rural areas of the U.S. can make this difficult.
Nearly 40% of last year’s congenital syphilis cases involved mothers who did not have prenatal care, according to the CDC.
If syphilis is diagnosed early in pregnancy, the threat of passing it to the baby can be removed by a single penicillin shot.
However, experts caution that the later into pregnancy the diagnosis is made, the more likely it is that multiple shots will be needed, and they must be completed at least 30 days before delivery.
Dr. Nina Ragunanthan, an esteemed OB/GYN at the Delta Health Center in Mound Bayou, Mississippi, has encountered numerous patients who have struggled to adhere to a prescribed three-shot regimen due to various impediments such as transportation, work commitments, and childcare responsibilities.
This predicament is not uncommon, as individuals who are earnestly attempting to undergo treatment may inadvertently miss a shot, thereby disrupting the continuity of their care.
The ramifications of such interruptions are profound, as incomplete treatment may impede the successful management of syphilis.
Compounding this issue is the scarcity of available shots, which poses a formidable challenge to health officials striving to curtail the prevalence of syphilis nationwide.
Furthermore, the utilization of the antibiotic doxycycline as an alternative treatment for non-pregnant patients is not without its own set of challenges, as the protracted 14- to 28-day treatment timeline presents difficulties in ensuring patient compliance and successful eradication of the infection.
These multifaceted obstacles underscore the urgent need for comprehensive strategies to address the complexities of syphilis treatment and prevention.
Pfizer, as the nation’s sole supplier of the penicillin shot, has recently experienced a shortage of this essential medication due to increased demand.
This shortage has raised concerns among healthcare professionals and patients who rely on penicillin for various medical conditions.
The company has acknowledged the issue and has stated that the shortage may not be resolved until next year.
This news has prompted discussions about the potential impact on patients’ access to necessary medication and the healthcare system as a whole.
It is crucial for Pfizer to address this shortage promptly and effectively to ensure that patients receive the treatment they need.
Additionally, it is important for the company to communicate transparently with healthcare providers and the public about the steps being taken to mitigate the shortage and prevent similar issues in the future.
The Centers for Disease Control and Prevention (CDC) has recently addressed concerns regarding a shortage of benzathine penicillin G, the recommended treatment for congenital syphilis.
Despite this shortage, the CDC has stated that it did not have an impact on the number of congenital syphilis cases reported in 2022.
Furthermore, the CDC has assured the public that it is not aware of any patients who were unable to receive their necessary treatment due to the shortage.
While the shortage of benzathine penicillin G is a concerning issue, the CDC’s reassurance provides some relief and confidence in the healthcare system’s ability to manage and address such challenges.
It is crucial for healthcare providers and authorities to continue monitoring the situation and taking proactive measures to ensure that patients receive the necessary treatment for congenital syphilis, despite the ongoing shortage of benzathine penicillin G.